What is Nipple-Sparing Mastectomy?
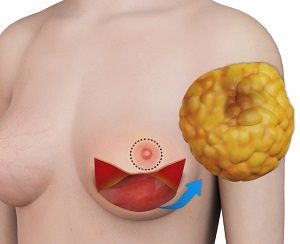
Mastectomy is a surgical procedure to remove one or both breasts to treat or prevent the spread of breast cancer. It usually involves the removal of breast tissue, the nipple, and areola. Nipple-sparing mastectomy is a variant of skin-sparing mastectomy that involves the removal of breast tissue, but leaves the nipple, areola, and breast skin intact. The main objective of the contemporary nipple-sparing mastectomy is to preserve the nipple-areolar complex (NAC) and skin covering with its blood supply while removing all breast tissue affected by cancer.
The use of nipple-sparing procedure has been increasing in prominence and has gained the acceptance and reputation of being a safe option with a low risk of cancer recurrence for patients with breast cancer. Nipple-sparing mastectomy is mostly followed by immediate breast reconstruction.
Some of the most common methods of immediate breast reconstruction include:
- Implant-Based Reconstruction: This method involves inserting a permanent implant that is filled with silicone gel or saline (saltwater) under the skin and muscle of the chest to create a new breast mound.
- Flap or Autologous Reconstruction: In this method, the patient’s own skin tissue is taken from another section of the body, such as the stomach, thigh, or buttocks, and used to create a new breast mound.
- Tissue Expanders: These are temporary implants that are placed behind the chest muscle to expand the area and make room for implant reconstruction. This method is mostly employed when the patient requires radiation therapy post mastectomy.
Indications for Nipple-Sparing Mastectomy
Nipple-sparing mastectomy is indicated for patients who wish to preserve the original appearance and shape of the breasts and nipple with superior cosmetic results. Some of the other indications for nipple-sparing mastectomy include:
- Women with no diagnosis of advanced breast cancer involving the skin or inflammatory breast cancer
- Women with a tumour that does not involve the nipple or tissue below the areola
- Women with a tumour that has been encircled by a clear boundary of cancer-free tissue
- Women seeking risk-reduction preventive surgery
- Women seeking therapeutic cancer surgery
Preparation for Nipple-Sparing Mastectomy
In general, preparation for nipple-sparing mastectomy may involve the following:
- A thorough examination by your doctor is performed to check for any medical issues that need to be addressed prior to the procedure.
- Depending on your medical history, social history, and age, you may need to undergo tests such as blood work and a mammogram to help detect any abnormalities that could threaten the safety of the procedure.
- You will be asked if you have allergies to medications, anaesthesia, or latex.
- Inform your doctor of any medications, vitamins, or supplements that you are taking.
- Refrain from taking any anti-inflammatory drugs, aspirin, or supplements, as they may increase the chance of bleeding.
- You should not consume any solids or liquids at least 8 hours prior to surgery.
- You may be instructed to shower with an antibacterial soap the night prior to surgery.
- Refrain from smoking pre- and post-procedure for a specific period of time, as this may hamper proper healing and increase your chances of areolar or nipple damage, tissue necrosis, and other complications.
- You will be given an opportunity to analyze before and after surgery pictures of patients’ who underwent nipple-sparing mastectomy.
- A written consent will be obtained from you after the procedure has been explained in detail.
Procedure for Nipple-Sparing Mastectomy
The procedure is performed under general anaesthesia. Your surgeon will discuss the best incisoon for you. The breast tissues are removed, leaving behind a natural skin pocket. The pocket may be immediately filled with your own body tissue or a breast implant, or a temporary tissue expander may be inserted, which maintains the space and size of the breast until breast reconstruction is performed. The implant is often supported with a mesh, which acts as an internal bra to hold the device in place. A drainage tube may be placed under each arm to drain excess fluid or blood. Finally, the incisions are closed with sutures and the breasts are wrapped with a waterproof dressing.
Post-Procedure Care and Recovery
Most patients can go home in a day or two after surgery if no complications are noted. The drains are usually removed in about a week or two following the surgery.
In general, postoperative care instructions and recovery involve the following:
- You may notice sensitivity, tenderness, swelling, and bruises over the reconstructed breast. Pain and anti-inflammatory medications are provided as needed.
- Your physician will also provide you with antibiotics to prevent the risk of infection.
- Refrain from any physical activity using your upper body or any strenuous activities for at least 4 to 6 weeks to promote healing.
- You will be able to have a shower in a day or two after surgery. A waterproof dressing will protect your surgical site.
- Your doctor will provide you with instructions on diet and wound care.
- You are recommended to wear a supportive bra for at least 2 days post procedure.
- Refrain from using anything too cold or too hot on your reconstructed breast skin as your breasts will lack normal sensation.
- You may need to take off from work for at least a week to facilitate recovery.
- You will be able to resume your normal activities within 4 to 6 weeks, but may have certain activity restrictions.
- You can drive within 2 to 3 weeks post surgery if you are not using pain medications and you are cleared by your doctor
- A periodic follow-up will be scheduled to monitor your overall progress.
Benefits of Nipple-Sparing Mastectomy
Some of the benefits of nipple-sparing mastectomy include:
- Minimal scarring
- Natural-looking breasts
- Helps to preserve aesthetics of the nipple
- Helps to preserve breast structure and form
- Better overall cosmetic outcome
- Improvement in self-image, self-esteem, and confidence
- Form-fitting clothes, sports bras, and swimsuits will feel and look better
Risks and Complications of Nipple-Sparing Mastectomy
Nipple-sparing mastectomy is a relatively safe procedure; however, as with any surgery, some risks and complications may occur, such as:
- Pain or tenderness
- Poor tissue healing
- Swelling/bruising
- Scar formation
- Damage to blood vessels and nerves
- Hematoma (accumulation of blood in the wound)
- Seroma (accumulation of clear fluid in the wound)
- Surgical site infection
- Anaesthetic reactions
- Numbness, tingling, or itching sensations
- Tissue necrosis requiring hyperbaric therapy or debridement
- Nipple loss or need for further surgery if the nipple has cancerous tissue.
